By Simon Booth
We live in age of predictive data. We have the ability to gather data in a certain area, over time, and use it to accurately predict outcomes.
This has been put to great effect in relation to personal injuries with tables such as the ODG evidence-based management guidelines. These guidelines outline recovery timeframes for specific injuries, along with required time off work and recommended treatment.
This use of evidence-based medicine enables healthcare providers to understand and accurately predict a person’s recovery time after specific injuries. Unfortunately, it appears that healthcare providers rarely apply this knowledge in relation to work related injuries.
It is well known that the approach of workers and healthcare providers to injury management and capacity relating to compensable injuries is often very different to their approach to non-compensable injuries.
Unfortunately, with work related injuries, capacity decisions often seem to lack any clinical justification. The stated capacity (or lack thereof) is more a reflection of the worker’s motivation or desire to stay off work, then the status of their compensable injury.
The reality is, where suitable duties are available, very few workers need time off work for an injury. Fewer still require extended absence from the workplace.
Despite this, the majority of first certificates provided by healthcare providers put the worker off work. This can result in workers with initially minor injuries having significant time off work. This in turn can result in the development of secondary issues, such as psychological conditions, weight gain and drug dependency. These factors then become the reason for ongoing incapacity.
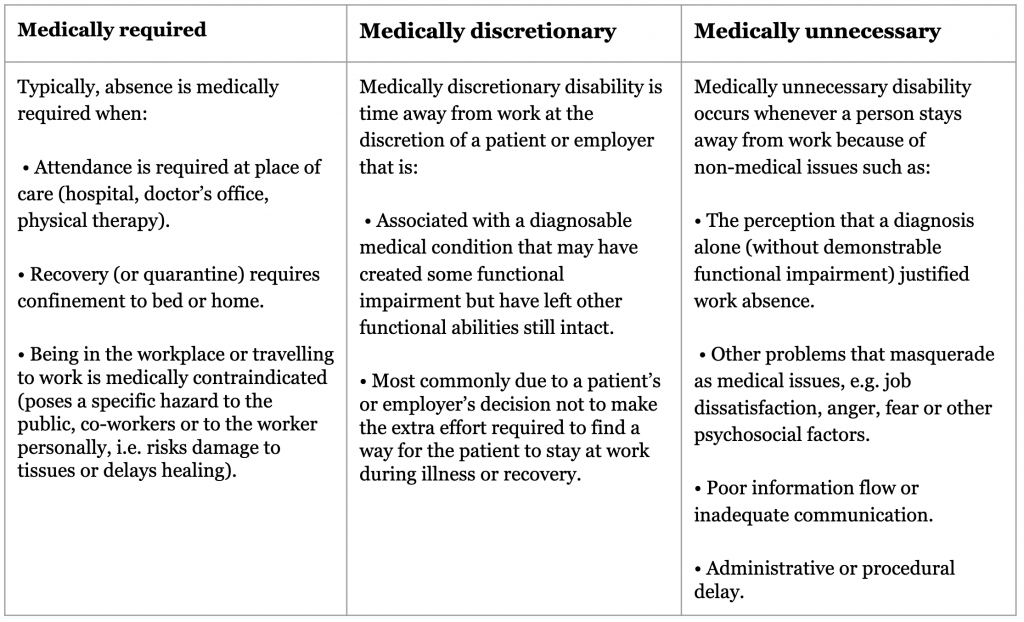
The Royal Australasian College of Physicians position statement on using evidence for better outcomes outlines the following table relating to work related medical disability.
Table: When is disability medically required, medically discretionary or medically unnecessary?
Source: The Royal Australasian College of Physicians, Australasian Faculty of Occupational and Environmental Medicine Policy on preventing work disability, Sydney 2010
This position statement clearly identifies that absence for work-related injury is only justified in a small percentage of cases. Many of the reasons that healthcare providers use to justify their assessment of incapacity do not pass the clinical justification test.
One of the ongoing issues is the lack of clinical distance exhibited by healthcare providers. Capacity decisions are often made from a position of advocacy not injury; a reflection of the healthcare provider’s opinion of the employer, based on the one-sided information provided by the worker.
This is highlighted in a study undertaken by Worksafe Victoria, which identified that:
- Only 41% of doctors believe that their patient’s employer wants their patient back at work.
- Only 27% believe that the employer will stick to the restrictions they outline on their certificate.
- Only 22% have confidence in the employer’s RTW Coordinator.
None of the points above is justification for certifying the worker as unfit for work. These are all issues that the table above places in the medically unnecessary column.
During my days as an occupational rehabilitation consultant, I sat in on more healthcare provider consultations with workers than I care to remember. During this time, I never witnessed a healthcare provider conduct a clinical assessment of the worker to determine their capacity for work.
Most commonly, a capacity decision was based solely on a discussion with the worker and the worker’s opinion:
- of their ability to return to work
- of the suitability of duties proposed by employer
Based on the deteriorating return to work figures across the country, I am confident that this approach has not changed.
The absence of clinical assessment and clinical justification does not assist the worker in recovery and return to work. To the contrary, this approach actually moves the worker from a state of recovery and return to work to that of disability and, potentially, malingering.
With the scheme and thereby the employer providing weekly benefits, the worker is rewarded for staying off work for extended periods.
“The return to work and workers’ compensation systems developed to meet the challenge of work disability sometimes contribute rather than ameliorate the difficulties faced by workers, families and employers.”1
For both workers and healthcare providers, the compensation associated with work related injuries removes the urgency and motivation for recovery that is present for non-work related injuries.
This results in health professionals certifying workers as having no capacity in situations where absence from work is medically unnecessary.
With this catastrophic failure by health professionals, it comes as no surprise that 75% of all first certificates provided by doctors state that the worker has no capacity for work.
People with non-work related injuries return to normal function considerably faster than people who sustain the exact same injury in the workplace. In addition, work related injuries and illness have significantly poorer overall health outcomes than non-work related conditions.
“The health outcomes for compensable conditions are worse than for similar non‐work‐related conditions.”1
The system needs to change to compensating workers solely for the incapacity relating to the injury. Where the timeframe relating to ability to return to work and/or recovery from injury has been reached, the healthcare providers should be required to provide clinical justification to support the ongoing incapacity for work.
This will require the agent/insurer communicating with the health professional after receipt of the certificate of capacity:
“You have diagnosed Worker X with ‘Diagnosis’. The ODG guidelines for this injury identify that the worker should be able to return to work on suitable duties by XX/XX/XXXX and should be fit for pre-injury duties by XX/XX/XXXX.
Please be advised that Worker X will only receive compensation for lost time relating to any certificates of incapacity beyond these dates, where:
- The worker’s employer is unable to provide suitable duties.
- There is clinical justification for ongoing incapacity.”
This necessitates a change at a legislative level. Previously we have seen little value placed on independent medical assessments outlining evidence-based clinical justification for their findings. The opinion of the worker’s healthcare provider has been given greater consideration despite a lack of clinical justification.
To address the deterioration of workers’ compensation schemes there must be a shift to focus on clinical assessment, clinical justification and evidence-based medicine.
Incapacity without clinical justification should not be compensable.
This approach is supported by The Royal Australasian College of Physicians. Their position statement identifies the need for a substantial overhaul of systems and legislation relating to workplace disability. Specifically, point 2 states:
“The use of evidence‐based medicine … should become standard practice and form the basis of return to work approaches.”
We need to stop thinking like the Victorian Ombudsman. Actions that disrupt the compensation cycle are neither immoral or unethical. To the contrary, these actions are mostly in the best interest of the worker. They are aimed at preventing long term disability associated with injuries where absence from work is medically unnecessary.
A new approach is needed. A system that allows and inadvertently encourages workers to remain off work will always be destined to fail.
It will fail financially.
It will fail the employers who must bear the cost of propping up the scheme.
Worst of all, it will fail the workers that it is meant to support. Sentencing many of them to unnecessary and undeserved long-term disability.
If you would like help with your Workers’ Compensation needs, today.
Sources
- The Royal Australasian College of Physicians, Australasian Faculty of Occupational and Environmental Medicine Policy on preventing work disability, Sydney 2010
https://www.racp.edu.au/docs/default-source/policy-and-adv/afoem/hbgw/helping-people-return-to-work-using-evidence-for-better-outcomes.pdf?sfvrsn=57ae3e1a_10 - WorkSafe Victoria https://www.worksafe.vic.gov.au/uncooperative-workers-doctor
- The role of general practitioners in worker rehabilitation — insights from the research. https://www.rtwmatters.org/article/articleG.php?id=2265&
- Victorian Ombudsman – WorkSafe 2: Follow-up investigation into the management of complex workers compensation claims (2019)
https://www.ombudsman.vic.gov.au/our-impact/investigation-reports/worksafe2-follow-up-investigation-into-the-management-of-complex-workers-compensation-claims/
Disclaimer: This article provides general advice and should not be considered legal advice or an insurance consultation. You should seek appropriate counsel for your own situation. In addition, this post is directed at people in Australia. If you are outside Australia, please be aware that the circumstances in your own country may be different.